What is immunoglobulin A (IgA) nephropathy?
IgA nephropathy, also known as Berger’s disease, is a kidney disease that occurs when IgA deposits build up in the kidneys, causing inflammation that damages kidney tissues. IgA is an antibody—a protein made by the immune system to protect the body from foreign substances such as bacteria or viruses. Most people with IgA nephropathy receive care from a nephrologist, a doctor who specializes in treating people with kidney disease.
How does IgA nephropathy affect the kidneys?
IgA nephropathy affects the kidneys by attacking the glomeruli. The glomeruli are sets of looping blood vessels in nephrons—the tiny working units of the kidneys that filter wastes and remove extra fluid from the blood. The buildup of IgA deposits inflames and damages the glomeruli, causing the kidneys to leak blood and protein into the urine. The damage may lead to scarring of the nephrons that progresses slowly over many years. Eventually, IgA nephropathy can lead to end-stage kidney disease, sometimes called ESRD, which means the kidneys no longer work well enough to keep a person healthy. When a person’s kidneys fail, he or she needs a transplant or blood-filtering treatments called dialysis.
More information is provided in the NIDDK health topic, Glomerular Diseases Overview.
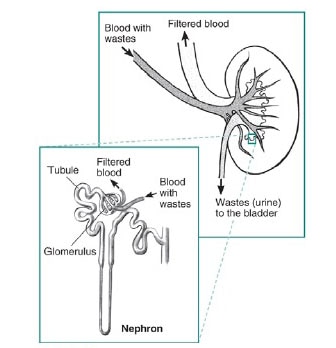
The glomeruli are sets of looping blood vessels in nephrons—the tiny working units of the kidneys that filter wastes and remove extra fluid from the blood.
What causes IgA nephropathy?
Scientists think that IgA nephropathy is an autoimmune kidney disease, meaning that the disease is due to the body’s immune system harming the kidneys.
People with IgA nephropathy have an increased blood level of IgA that contains less of a special sugar, galactose, than normal. This galactose-deficient IgA is considered “foreign” by other antibodies circulating in the blood. As a result, these other antibodies attach to the galactose-deficient IgA and form a clump. This clump is also called an immune complex. Some of the clumps become stuck in the glomerulus of the nephron and cause inflammation and damage.
For some people, IgA nephropathy runs in families. Scientists have recently found several genetic markers that may play a role in the development of the disease. IgA nephropathy may also be related to respiratory or intestinal infections and the immune system’s response to these infections.
How common is IgA nephropathy and who is more likely to get the disease?
IgA nephropathy is one of the most common kidney diseases, other than those caused by diabetes or high blood pressure.1
IgA nephropathy can occur at any age, although the first evidence of kidney disease most frequently appears when people are in their teens to late 30s.2 IgA nephropathy in the United States is twice as likely to appear in men than in women.3 While found in people all over the world, IgA nephropathy is more common among Asians and Caucasians.4
A person may be more likely to develop IgA nephropathy if
- he or she has a family history of IgA nephropathy or IgA vasculitis—a disease that causes small blood vessels in the body to become inflamed and leak
- he is a male in his teens to late 30s
- he or she is Asian or Caucasian
What are the signs and symptoms of IgA nephropathy?
In its early stages, IgA nephropathy may have no symptoms; it can be silent for years or even decades. Once symptoms appear, the most common one is hematuria, or blood in the urine. Hematuria can be a sign of damaged glomeruli. Blood in the urine may appear during or soon after a cold, sore throat, or other respiratory infection. The amount of blood may be
- visible with the naked eye. The urine may turn pink or the color of tea or cola. Sometimes a person may have dark or bloody urine.
- so small that it can only be detected using special medical tests.
Another symptom of IgA nephropathy is albuminuria—when a person’s urine contains an increased amount of albumin, a protein typically found in the blood, or large amounts of protein in the urine. Albumin is the main protein in the blood. Healthy kidneys keep most proteins in the blood from leaking into the urine. However, when the glomeruli are damaged, large amounts of protein leak out of the blood into the urine.
When albumin leaks into the urine, the blood loses its capacity to absorb extra fluid from the body. Too much fluid in the body may cause edema, or swelling, usually in the legs, feet, or ankles and less often in the hands or face. Foamy urine is another sign of albuminuria. Some people with IgA nephropathy have both hematuria and albuminuria.
After 10 to 20 years with IgA nephropathy, about 20 to 40 percent of adults develop end-stage kidney disease.5 Signs and symptoms of end-stage kidney disease may include
- high blood pressure
- little or no urination
- edema
- feeling tired
- drowsiness
- generalized itching or numbness
- dry skin
- headaches
- weight loss
- appetite loss
- nausea
- vomiting
- sleep problems
- trouble concentrating
- darkened skin
- muscle cramps
What are the complications of IgA nephropathy?
Complications of IgA nephropathy include
- high blood pressure
- acute kidney failure—sudden and temporary loss of kidney function
- chronic kidney failure—reduced kidney function over a period of time
- nephrotic syndrome—a collection of symptoms that indicate kidney damage; symptoms include albuminuria, lack of protein in the blood, and high blood cholesterol levels
- heart or cardiovascular problems
- Henoch-Schönlein purpura
More information is provided in the NIDDK health topics, Kidney Disease and Kidney Failure.
How is kidney disease diagnosed?
A health care provider diagnoses kidney disease with
- a medical and family history
- a physical exam
- urine tests
- a blood test
Medical and Family History
Taking a medical and family history may help a health care provider diagnose kidney disease.
Physical Exam
A physical exam may help diagnose kidney disease. During a physical exam, a health care provider usually
- measures the patient’s blood pressure
- examines the patient’s body for swelling
Urine Tests
Dipstick test for albumin and blood. A dipstick test performed on a urine sample can detect the presence of albumin and blood. The patient provides a urine sample in a special container in a health care provider’s office or a commercial facility. A nurse or technician can test the sample in the same location, or he or she can send it to a lab for analysis. The test involves placing a strip of chemically treated paper, called a dipstick, into the patient’s urine sample. Patches on the dipstick change color when albumin or blood is present in urine.
Urine albumin-to-creatinine ratio. A health care provider uses this measurement, which compares the amount of albumin with the amount of creatinine in a urine sample, to estimate 24-hour albumin excretion. A patient may have chronic kidney disease if the urine albumin-to-creatinine ratio is greater than 30 milligrams (mg) of albumin for each gram (g) of creatinine (30 mg/g). This measurement is also called UACR.
Blood Test
A blood test involves having blood drawn at a health care provider’s office or a commercial facility and sending the sample to a lab for analysis. A health care provider may order a blood test to estimate how much blood a patient’s kidneys filter each minute—a measurement called the estimated glomerular filtration rate (eGFR). Depending on the results, the test can indicate the following:
- eGFR of 60 or above is in the normal range
- eGFR below 60 may indicate kidney disease
- eGFR of 15 or below may indicate kidney failure
How is IgA nephropathy diagnosed?
Currently, health care providers do not use blood or urine tests as reliable ways to diagnose IgA nephropathy; therefore, the diagnosis of IgA nephropathy requires a kidney biopsy.
A kidney biopsy is a procedure that involves taking a small piece of kidney tissue for examination with a microscope. A health care provider performs a kidney biopsy in a hospital or an outpatient center with light sedation and a local anesthetic. The health care provider uses imaging techniques such as ultrasound or a computerized tomography scan to guide the biopsy needle into the kidney. A pathologist—a doctor who specializes in examining tissues to diagnose diseases—examines the kidney tissue with a microscope. Only a biopsy can show the IgA deposits in the glomeruli. The biopsy can also show how much kidney damage has already occurred. The biopsy results can help the health care provider determine the best course of treatment.
How is IgA nephropathy treated?
Researchers have not yet found a specific cure for IgA nephropathy. Once the kidneys are scarred, they cannot be repaired. Therefore, the ultimate goal of IgA nephropathy treatment is to prevent or delay end-stage kidney disease. A health care provider may prescribe medications to
- control a person’s blood pressure and slow the progression of kidney disease
- remove extra fluid from a person’s blood
- control a person’s immune system
- lower a person’s blood cholesterol levels
Control Blood Pressure and Slow Progression of Kidney Disease
People with IgA nephropathy that is causing high blood pressure may need to take medications that lower blood pressure and can also significantly slow the progression of kidney disease. Two types of blood pressure-lowering medications—angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARBs)—have proven effective in slowing the progression of kidney disease. Many people require two or more medications to control their blood pressure. A person may also need beta-blockers, calcium channel blockers, and other blood pressure medications.
Remove Extra Fluid
A health care provider may prescribe a diuretic, a medication that helps the kidneys remove extra fluid from the blood. Removing the extra fluid can improve the control of blood pressure. Taking a diuretic along with an ACE inhibitor or an ARB often increases the effectiveness of these medications.
Control the Immune System
Health care providers sometimes use medications to control a person’s immune system. Since inflammation is the immune system’s normal response, controlling the immune system can decrease inflammation. Health care providers may prescribe the following medications:
- corticosteroids, such as prednisone
- cyclophosphamide
Lower Blood Cholesterol Levels
People with IgA nephropathy may develop high blood cholesterol levels. Cholesterol is a type of fat found in the body’s cells, in blood, and in many foods. People who take medications for high blood cholesterol levels can lower their blood cholesterol levels. A health care provider may prescribe one of several cholesterol-lowering medications called statins.
How can a person prevent IgA nephropathy?
Researchers have not found a way to prevent IgA nephropathy. People with a family history of IgA nephropathy should talk with their health care provider to find out what steps they can take to keep their kidneys healthy, such as controlling their blood pressure and keeping their blood cholesterol at healthy levels.
Eating, Diet, and Nutrition
Researchers have not found that eating, diet, and nutrition play a role in causing or preventing IgA nephropathy. Health care providers may recommend that people with kidney disease, such as IgA nephropathy, make dietary changes such as
- limiting dietary sodium, often from salt, to help reduce edema and lower blood pressure
- decreasing liquid intake to help reduce edema and lower blood pressure
- eating a diet low in saturated fat and cholesterol to help control high levels of lipids, or fats, in the blood
Health care providers may also recommend that people with kidney disease eat moderate or reduced amounts of protein, although the benefit of reducing protein in a person’s diet is still being researched. Proteins break down into waste products the kidneys must filter from the blood. Eating more protein than the body needs may burden the kidneys and cause kidney function to decline faster. However, protein intake that is too low may lead to malnutrition, a condition that occurs when the body does not get enough nutrients. People with kidney disease on a restricted protein diet should receive blood tests that can show nutrient levels.
Some researchers have shown that fish oil supplements containing omega-3 fatty acids may slow kidney damage in some people with kidney disease by lowering blood pressure. Omega-3 fatty acids may help reduce inflammation and slow kidney damage due to IgA nephropathy. To help ensure coordinated and safe care, people should discuss their use of complementary and alternative medical practices, including their use of dietary supplements and probiotics, with their health care provider. Read more at nccih.nih.gov/health/supplements NIH external link.
People with IgA nephropathy should talk with a health care provider about dietary changes to best manage their individual needs.
Points to Remember
- Immunoglobulin A (IgA) nephropathy, also known as Berger’s disease, is a kidney disease that occurs when IgA deposits build up in the kidneys, causing inflammation that damages kidney tissues.
- Scientists think that IgA nephropathy is an autoimmune kidney disease, meaning that the disease is due to the body’s immune system attacking tissues in the kidney.
- IgA nephropathy is one of the most common kidney diseases, other than those caused by diabetes or high blood pressure.
- In its early stages, IgA nephropathy may have no symptoms; it can be silent for years or even decades.
- Once symptoms appear, the most common one is hematuria, or blood in the urine.
- Another symptom of IgA nephropathy is albuminuria—when a person’s urine contains an increased amount of albumin, a protein typically found in the blood, or large amounts of protein in the urine.
- Currently, health care providers do not use blood or urine tests as reliable ways to diagnose IgA nephropathy; therefore, the diagnosis of IgA nephropathy requires a kidney biopsy.
- Researchers have not yet found a specific cure for IgA nephropathy.
Clinical Trials
- The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) and other components of the National Institutes of Health (NIH) conduct and support research into many diseases and conditions.
What are clinical trials, and are they right for you?
Clinical trials are part of clinical research and at the heart of all medical advances. Clinical trials look at new ways to prevent, detect, or treat disease. Researchers also use clinical trials to look at other aspects of care, such as improving the quality of life for people with chronic illnesses. Find out if clinical trials are right for you NIH external link.
What clinical trials are open?
Clinical trials that are currently open and are recruiting can be viewed at www.ClinicalTrials.gov NIH external link.