What Is Chronic Kidney Disease?
In this section:
- How common is CKD?
- Who is more likely to develop CKD?
- What are the symptoms of CKD?
- Does CKD cause other health problems?
- How can CKD affect my day-to-day life?
- Will my kidneys get better?
- What happens if my kidneys fail?
Chronic kidney disease (CKD) means your kidneys are damaged and can’t filter blood the way they should. The disease is called “chronic” because the damage to your kidneys happens slowly over a long period of time. This damage can cause wastes to build up in your body. CKD can also cause other health problems.
The kidneys’ main job is to filter extra water and wastes out of your blood to make urine. To keep your body working properly, the kidneys balance the salts and minerals—such as calcium, phosphorus, sodium, and potassium—that circulate in the blood. Your kidneys also make hormones that help control blood pressure, make red blood cells, and keep your bones strong.
Kidney disease often can get worse over time and may lead to kidney failure. If your kidneys fail, you will need dialysis or a kidney transplant to maintain your health.
The sooner you know you have kidney disease, the sooner you can make changes to protect your kidneys.
More information is provided in the NIDDK health topic, The Kidneys and How They Work.
Watch a video about what the kidneys do.
How common is CKD?
CKD is common among adults in the United States. More than 37 million American adults may have CKD.1
Who is more likely to develop CKD?
You are at risk for kidney disease if you have
- Diabetes. Diabetes is the leading cause of CKD. High blood glucose, also called blood sugar, from diabetes can damage the blood vessels in your kidneys. Almost 1 in 3 people with diabetes has CKD.1
- High blood pressure. High blood pressure is the second leading cause of CKD. Like high blood glucose, high blood pressure also can damage the blood vessels in your kidneys. Almost 1 in 5 adults with high blood pressure has CKD.1
- Heart disease. Research shows a link between kidney disease and heart disease. People with heart disease are at higher risk for kidney disease, and people with kidney disease are at higher risk for heart disease. Researchers are working to better understand the relationship between kidney disease and heart disease.
- Family history of kidney failure. If your mother, father, sister, or brother has kidney failure, you are at risk for CKD. Kidney disease tends to run in families. If you have kidney disease, encourage family members to get tested. Use tips from the family health reunion guide and speak with your family during special gatherings.
Your chances of having kidney disease increase with age.1 The longer you have had diabetes, high blood pressure, or heart disease, the more likely that you will have kidney disease.
African Americans, Hispanics, and American Indians tend to have a greater risk for CKD.2 The greater risk is due mostly to higher rates of diabetes and high blood pressure among these groups. Scientists are studying other possible reasons for this increased risk.
Watch a video about kidney disease risk
If you are at risk for kidney disease, learn ways to prevent kidney disease.
What are the symptoms of CKD?
Early CKD may not have any symptoms
You may wonder how you can have CKD and feel fine. Our kidneys have a greater capacity to do their job than is needed to keep us healthy. For example, you can donate one kidney and remain healthy. You can also have kidney damage without any symptoms because, despite the damage, your kidneys are still doing enough work to keep you feeling well. For many people, the only way to know if you have kidney disease is to get your kidneys checked with blood and urine tests.
As kidney disease gets worse, a person may have swelling, called edema. Edema happens when the kidneys can’t get rid of extra fluid and salt. Edema can occur in the legs, feet, or ankles, and less often in the hands or face.
Symptoms of advanced CKD
- chest pain
- dry skin
- itching or numbness
- feeling tired
- headaches
- increased or decreased urination
- loss of appetite
- muscle cramps
- nausea
- shortness of breath
- sleep problems
- trouble concentrating
- vomiting
- weight loss
People with CKD can also develop anemia, bone disease, and malnutrition.
Does CKD cause other health problems?
Kidney disease can lead to other health problems, such as heart disease. If you have kidney disease, it increases your chances of having a stroke or heart attack.
High blood pressure can be both a cause and a result of kidney disease. High blood pressure damages your kidneys, and damaged kidneys don’t work as well to help control your blood pressure.
If you have CKD, you also have a higher chance of having a sudden change in kidney function caused by illness, injury, or certain medicines. This is called acute kidney injury (AKI).
How can CKD affect my day-to-day life?
Many people are afraid to learn that they have kidney disease because they think that all kidney disease leads to dialysis. However, most people with kidney disease will not need dialysis. If you have kidney disease, you can continue to live a productive life, work, spend time with friends and family, stay physically active, and do other things you enjoy. You may need to change what you eat and add healthy habits to your daily routine to help you protect your kidneys.
Will my kidneys get better?
Kidney disease is often “progressive”, which means it gets worse over time. The damage to your kidneys causes scars and is permanent.
You can take steps to protect your kidneys, such as managing your blood pressure and your blood glucose, if you have diabetes.
What happens if my kidneys fail?
Kidney failure means that your kidneys have lost most of their ability to function—less than 15 percent of normal kidney function. If you have kidney failure, you will need treatment to maintain your health. Learn more about what happens if your kidneys fail.
References
Causes of Chronic Kidney Disease
Diabetes and high blood pressure are the most common causes of chronic kidney disease (CKD). Your health care provider will look at your health history and may do tests to find out why you have kidney disease. The cause of your kidney disease may affect the type of treatment you receive.
Diabetes
Too much glucose, also called sugar, in your blood damages your kidneys’ filters. Over time, your kidneys can become so damaged that they no longer do a good job filtering wastes and extra fluid from your blood.
Often, the first sign of kidney disease from diabetes is protein in your urine. When the filters are damaged, a protein called albumin, which you need to stay healthy, passes out of your blood and into your urine. A healthy kidney doesn’t let albumin pass from the blood into the urine.
Diabetic kidney disease is the medical term for kidney disease caused by diabetes.
High blood pressure
High blood pressure can damage blood vessels in the kidneys so they don’t work as well. If the blood vessels in your kidneys are damaged, your kidneys may not work as well to remove wastes and extra fluid from your body. Extra fluid in the blood vessels may then raise blood pressure even more, creating a dangerous cycle.
More information is provided in the NIDDK health topic, High Blood Pressure and Kidney Disease.
Other causes of kidney disease
Other causes of kidney disease include
- a genetic disorder that causes many cysts to grow in the kidneys, polycystic kidney disease (PKD).
- an infection
- a drug that is toxic to the kidneys
- a disease that affects the entire body, such as diabetes or lupus NIH external link. Lupus nephritis is the medical name for kidney disease caused by lupus
- IgA glomerulonephritis
- disorders in which the body’s immune system attacks its own cells and organs, such as Anti-GBM (Goodpasture’s) disease
- heavy metal poisoning, such as lead poisoning NIH external link
- rare genetic conditions, such as Alport syndrome NIH external link
- hemolytic uremic syndrome in children
- IgA vasculitis
- renal artery stenosis
Chronic Kidney Disease Tests & Diagnosis
How can I tell if I have kidney disease?
Early kidney disease usually doesn’t have any symptoms. Testing is the only way to know how well your kidneys are working. Get checked for kidney disease if you have
- diabetes
- high blood pressure
- heart disease
- a family history of kidney failure
If you have diabetes, get checked every year. If you have high blood pressure, heart disease, or a family history of kidney failure, talk with your health care provider about how often you should get tested. The sooner you know you have kidney disease, the sooner you can get treatment to help protect your kidneys.
What tests do doctors use to diagnose and monitor kidney disease?
To check for kidney disease, health care providers use
- a blood test that checks how well your kidneys are filtering your blood, called GFR. GFR stands for glomerular filtration rate.
- a urine test to check for albumin. Albumin is a protein that can pass into the urine when the kidneys are damaged.
If you have kidney disease, your health care provider will use the same two tests to help monitor your kidney disease and make sure your treatment plan is working.
Watch a video on how to check for kidney disease.
Blood test for GFR
Your health care provider will use a blood test to check your kidney function. The results of the test mean the following:
- a GFR of 60 or more is in the normal range. Ask your health care provider when your GFR should be checked again.
- a GFR of less than 60 may mean you have kidney disease. Talk with your health care provider about how to keep your kidney health at this level.
- a GFR of 15 or less is called kidney failure. Most people below this level need dialysis or a kidney transplant. Talk with your health care provider about your treatment options.
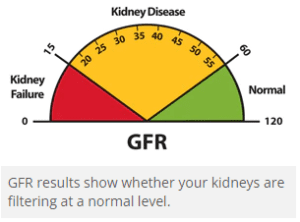 You can’t raise your GFR, but you can try to keep it from going lower. Learn more about what you can do to keep your kidneys healthy.Creatinine. Creatinine is a waste product from the normal breakdown of muscles in your body. Your kidneys remove creatinine from your blood. Providers use the amount of creatinine in your blood to estimate your GFR. As kidney disease gets worse, the level of creatinine goes up.
You can’t raise your GFR, but you can try to keep it from going lower. Learn more about what you can do to keep your kidneys healthy.Creatinine. Creatinine is a waste product from the normal breakdown of muscles in your body. Your kidneys remove creatinine from your blood. Providers use the amount of creatinine in your blood to estimate your GFR. As kidney disease gets worse, the level of creatinine goes up.
Urine Test for Albumin
If you are at risk for kidney disease, your provider may check your urine for albumin.
Albumin is a protein found in your blood. A healthy kidney doesn’t let albumin pass into the urine. A damaged kidney lets some albumin pass into the urine. The less albumin in your urine, the better. Having albumin in the urine is called albuminuria.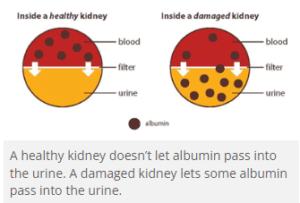
A health care provider can check for albumin in your urine in two ways:
Dipstick test for albumin. A provider uses a urine sample to look for albumin in your urine. You collect the urine sample in a container in a health care provider’s office or lab. For the test, a provider places a strip of chemically treated paper, called a dipstick, into the urine. The dipstick changes color if albumin is present in the urine.
Urine albumin-to-creatinine ratio (UACR). This test measures and compares the amount of albumin with the amount of creatinine in your urine sample. Providers use your UACR to estimate how much albumin would pass into your urine over 24 hours. A urine albumin result of
- 30 mg/g or less is normal
- more than 30 mg/g may be a sign of kidney disease
If you have albumin in your urine, your provider may want you to repeat the urine test one or two more times to confirm the results. Talk with your provider about what your specific numbers mean for you.
If you have kidney disease, measuring the albumin in your urine helps your provider know which treatment is best for you. A urine albumin level that stays the same or goes down may mean that treatments are working.
How do I know if my kidney disease is getting worse?
You can keep track of your test results (PDF, 262 KB) over time. You can tell that your treatments are working if your
- GFR stays the same
- urine albumin stays the same or goes down
Your health care provider will work with you to manage your kidney disease.
Managing Chronic Kidney Disease
If you have chronic kidney disease (CKD), you can take steps to protect your kidneys from more damage.
The sooner you know you have kidney disease, the better. The steps you take to protect your kidneys from damage also may help prevent heart disease—and improve your health overall. Making these changes when you have no symptoms may be hard, but it’s worthwhile.
Ten ways to manage kidney disease
Control your blood pressure
The most important step you can take to treat kidney disease is to control your blood pressure. High blood pressure can damage your kidneys. You can protect your kidneys by keeping your blood pressure at or less than the goal set by your health care provider. For most people, the blood pressure goal is less than 140/90 mm Hg.
Work with your health care provider to develop a plan to meet your blood pressure goals. Steps you can take to meet your blood pressure goals may include eating heart-healthy and low-sodium meals, quitting smoking, being active, getting enough sleep, and taking your medicines as prescribed.
Meet your blood glucose goal if you have diabetes
To reach your blood glucose goal, check your blood glucose level regularly. Use the results to guide decisions about food, physical activity, and medicines. Ask your health care provider how often you should check your blood glucose level.
Your health care provider will also test your A1C. The A1C is a blood test that measures your average blood glucose level over the past 3 months. This test is different from the blood glucose checks you do regularly. The higher your A1C number, the higher your blood glucose levels have been during the past 3 months. Stay close to your daily blood glucose numbers to help you meet your A1C goal.
The A1C goal for many people with diabetes is below 7 percent. Ask your health care provider what your goal should be. Reaching your goal numbers will help you protect your kidneys. Learn more about how to manage diabetes.
Work with your health care team to monitor your kidney health
The tests that health care providers use to test for kidney disease can also be used to track changes to kidney function and damage. Kidney disease tends to get worse over time. Each time you get checked, ask your provider how the test results compare to the last results. Your goals will be to
- keep your GFR the same
- keep your urine albumin the same or lower
Your health care provider will also check your blood pressure and, if you have diabetes, your A1C level, to make sure you are meeting your blood pressure and blood glucose goals.
Bring this document to your appointment to help keep track of your kidney test results (PDF, 262 KB) .
How can I prepare for visits with my health care provider?
The more you plan for your visits, the more you will be able to learn about your health and treatment options.
Make a list of questions
It’s normal to have a lot of questions. Write down your questions as you think of them so that you can remember everything you want to ask when you see your health care provider. You may want to ask about what tests are being done, what test results mean, or the changes you need to make to your diet and medicines.
Sample questions to ask your provider for people with kidney disease
About your tests
- What is my GFR? What does that mean?
- Has my GFR changed since last time?
- What is my urine albumin? What does it mean?
- Has my urine albumin changed since the last time it was checked?
- Is my kidney disease getting worse?
- Is my blood pressure where it needs to be?
About treatment and self-care
- What can I do to keep my disease from getting worse?
- Do any of my medicines or doses need to be changed?
- What time of day should I take each of my medicines?
- Do I need to change what I eat?
- Will you refer me to a dietitian for diet counseling?
- When will I need to see a nephrologist (kidney specialist)?
- Do I need to worry about dialysis or a kidney transplant?
- What do I need to do to protect my veins?
About complications
- What other health problems may I face because of my kidney disease?
- Should I be looking for any symptoms? If so, what are they?
Bring a friend or relative with you for support
A trusted friend or family member can take notes, ask questions you may not have thought of, offer support, and help remember what the provider said during the visit. Talk ahead of time about what you want to get out of the visit and the role you would like your friend or relative to play.
Who is part of my health care team?
The following health care providers may be part of the health care team involved in your treatment:
Primary care provider. Your primary care provider (PCP)—doctor, nurse practitioner, or physician assistant—is the person you see for routine medical visits. Your PCP may monitor your kidney health and help you manage your diabetes and high blood pressure. A PCP also prescribes medicines and may refer you to specialists.
Nurse. A nurse may help with your treatment and teach you about monitoring and treating kidney disease, as well as managing your health conditions. Some nurses specialize in kidney disease.
Registered dietitian. A registered dietitian is a food and nutrition expert who helps people create a healthy eating plan when they have a health condition such as kidney disease. Dietitians can help you by creating an eating plan based on how your kidneys are doing. “Renal dietitians” often work in dialysis centers and are specially trained to work with people with kidney failure.
Diabetes educator. A diabetes educator teaches people with diabetes how to manage their disease and handle diabetes-related problems.
Pharmacist. A pharmacist educates you about your medicines and fills your prescriptions. An important job for the pharmacist is to review all of your medicines, including over-the-counter (OTC) medicines, and supplements, to avoid unsafe combinations and side effects.
Social worker. When you are close to needing dialysis, you may have a chance to meet with a social worker. A dialysis social worker helps people and their families deal with the life changes and costs that come with having kidney disease and kidney failure. A dialysis social worker also can help people with kidney failure apply for help to cover treatment costs.
Nephrologist. A nephrologist is a doctor who is a kidney specialist. Your PCP may refer you to a nephrologist if you have a complicated case of kidney disease, your kidney disease is quickly getting worse, or your kidney disease is advanced.
Take medicines as prescribed
Many people with CKD take medicines prescribed to lower blood pressure, control blood glucose, and lower cholesterol.
Two types of blood pressure medicines, ACE inhibitors and ARBs, may slow kidney disease and delay kidney failure, even in people who don’t have high blood pressure. The names of these medicines end in –pril or –sartan.
Many people need to take two or more medicines for their blood pressure. You may also need to take a diuretic, sometimes called a water pill. The aim is to meet your blood pressure goal. These medicines may work better if you limit your salt intake.
Know that your medicines may change over time
Your health care provider may change your medicines as your kidney disease gets worse. Your kidneys don’t filter as well as they did in the past, and this can cause an unsafe buildup of medicines in your blood. Some medicines can also harm your kidneys. As a result, your provider may tell you to
- take a medicine less often or take a smaller dose
- stop taking a medicine or switch to a different one
Your pharmacist and health care provider need to know about all the medicines you take, including OTC medicines, vitamins, and supplements.
Be careful about the over-the-counter medicines you take
If you take OTC or prescription medicines for headaches, pain, fever, or colds, you may be taking nonsteroidal anti-inflammatory drugs (NSAIDs). NSAIDs include commonly used pain relievers and cold medicines that can damage your kidneys and lead to acute kidney injury, especially in those with kidney disease, diabetes, and high blood pressure.
Ibuprofen NIH external link and naproxen NIH external link are NSAIDs. NSAIDs are sold under many different brand names, so ask your pharmacist or health care provider if the medicines you take are safe to use.
You also can look for NSAIDs on Drug Facts labels like the one below:
Watch a video explaining how NSAIDs can harm your kidneys
If you have been taking NSAIDs regularly to control chronic pain, you may want to ask your health care provider about other ways to treat pain, such as meditation NIH external link or other relaxation techniques. You can read more about pain management at the NIH National Center for Complementary and Integrative Health website
Tips for managing your medicines
The next time you pick up a prescription or buy an OTC medicine or supplement, ask your pharmacist how the product may
- affect your kidneys
- affect other medicines you take
Fill your prescriptions at only one pharmacy or pharmacy chain so your pharmacist can
- keep track of your medicines and supplements
- check for harmful interactions
Keep track of your medicines and supplements:
- Keep an up-to-date list of your medicines and supplements in your wallet. Take your list with you, or bring all of your medicine bottles, to all health care visits.
Work with a dietitian to develop a meal plan
What you eat and drink can help you
- protect your kidneys
- reach your blood pressure and blood glucose goals
- prevent or delay health problems caused by kidney disease
As your kidney disease gets worse, you may need to make more changes to what you eat and drink.
A dietitian who knows about kidney disease can work with you to create a meal plan that includes foods that are healthy for you and that you enjoy eating. Cooking and preparing your food from scratch can help you eat healthier.
Nutrition counseling from a registered dietitian to help meet your medical or health goals is called medical nutrition therapy (MNT). If you have diabetes or kidney disease and a referral from your primary care provider, your health insurance may cover MNT. If you qualify for Medicare, MNT is covered.
Your health care provider may be able to refer you to a dietitian. You can also find a registered dietitian External link online through the Academy of Nutrition and Dietetics. Work closely with your dietitian to learn to eat right for CKD.
Make physical activity part of your routine
Be active for 30 minutes or more on most days. Physical activity can help you reduce stress, manage your weight, and achieve your blood pressure and blood glucose goals. If you are not active now, ask your health care provider about the types and amounts of physical activity that are right for you.
View physical activity and weight-management resources to help you get and stay motivated.
Aim for a healthy weight
Being overweight makes your kidneys work harder and may damage your kidneys. The NIH Body Weight Planner is an online tool to help you tailor your calorie and physical activity plans to achieve and stay at a healthy weight.
Get enough sleep
Aim for 7 to 8 hours of sleep each night. Getting enough sleep is important to your overall physical and mental health and can help you meet your blood pressure and blood glucose goals. You can take steps to improve your sleep habits NIH external link.
Stop smoking
Cigarette smoking can make kidney damage worse. Quitting smoking may help you meet your blood pressure goals, which is good for your kidneys, and can lower your chances of having a heart attack or stroke. For tips on quitting, go to Smokefree.gov.
Find healthy ways to cope with stress and depression
Long-term stress can raise your blood pressure and your blood glucose and lead to depression. Some of the steps that you are taking to manage your kidney disease are also healthy ways to cope with stress. For example, physical activity and sleep help reduce stress. Listening to your favorite music, focusing on something calm or peaceful, or meditating may also help you. Learn more about healthy ways to cope with stress NIH external link.
Depression is common among people with a chronic, or long-term, illness NIH external link. Depression can make it harder to manage your kidney disease. Ask for help if you feel down. Seek help from a mental health professional. Talking with a support group, clergy member, friend, or family member who will listen to your feelings may help.
Eating Right for Chronic Kidney Disease
You may need to change what you eat to manage your chronic kidney disease (CKD). Work with a registered dietitian to develop a meal plan that includes foods that you enjoy eating while maintaining your kidney health.
The steps below will help you eat right as you manage your kidney disease. The first three steps (1-3) are important for all people with kidney disease. The last two steps (4-5) may become important as your kidney function goes down.
The first steps to eating right
Step 1: Choose and prepare foods with less salt and sodium
Why? To help control your blood pressure. Your diet should contain less than 2,300 milligrams of sodium each day.
- Buy fresh food often. Sodium (a part of salt) is added to many prepared or packaged foods you buy at the supermarket or at restaurants.
- Cook foods from scratch instead of eating prepared foods, “fast” foods, frozen dinners, and canned foods that are higher in sodium. When you prepare your own food, you control what goes into it.
- Use spices, herbs, and sodium-free seasonings in place of salt.
- Check for sodium on the Nutrition Facts label of food packages. A Daily Value of 20 percent or more means the food is high in sodium.
- Try lower-sodium versions of frozen dinners and other convenience foods.
- Rinse canned vegetables, beans, meats, and fish with water before eating.
Look for food labels with words like sodium free or salt free; or low, reduced, or no salt or sodium; or unsalted or lightly salted.
Step 2: Eat the right amount and the right types of protein
Why? To help protect your kidneys. When your body uses protein, it produces waste. Your kidneys remove this waste. Eating more protein than you need may make your kidneys work harder.
- Eat small portions of protein foods.
- Protein is found in foods from plants and animals. Most people eat both types of protein. Talk to your dietitian about how to choose the right combination of protein foods for you.
Animal-protein foods:
- Chicken
- Fish
- Meat
- Eggs
- Dairy
A cooked portion of chicken, fish, or meat is about 2 to 3 ounces or about the size of a deck of cards. A portion of dairy foods is ½ cup of milk or yogurt, or one slice of cheese.
Plant-protein foods:
- Beans
- Nuts
- Grains
A portion of cooked beans is about ½ cup, and a portion of nuts is ¼ cup. A portion of bread is a single slice, and a portion of cooked rice or cooked noodles is ½ cup.
Step 3: Choose foods that are healthy for your heart
Why? To help keep fat from building up in your blood vessels, heart, and kidneys.
- Grill, broil, bake, roast, or stir-fry foods, instead of deep frying.
- Cook with nonstick cooking spray or a small amount of olive oil instead of butter.
- Trim fat from meat and remove skin from poultry before eating.
- Try to limit saturated and trans fats. Read the food label.
Heart-healthy foods:
- Lean cuts of meat, such as loin or round
- Poultry without the skin
- Fish
- Beans
- Vegetables
- Fruits
- Low-fat or fat-free milk, yogurt, and cheese
Learn more about heart-healthy eating
Limit alcohol
Drink alcohol only in moderation: no more than one drink per day if you are a woman, and no more than two if you are a man. Drinking too much alcohol can damage the liver, heart, and brain and cause serious health problems. Ask your health care provider how much alcohol you can drink safely.
The next steps to eating right
As your kidney function goes down, you may need to eat foods with less phosphorus and potassium. Your health care provider will use lab tests to check phosphorus and potassium levels in your blood, and you can work with your dietitian to adjust your meal plan. More information is provided in the NIDDK health topic, Nutrition for Advanced Chronic Kidney Disease.
Step 4: Choose foods and drinks with less
phosphorus
Why? To help protect your bones and blood vessels. When you have CKD, phosphorus can build up in your blood. Too much phosphorus in your blood pulls calcium from your bones, making your bones thin, weak, and more likely to break. High levels of phosphorus in your blood can also cause itchy skin, and bone and joint pain.
- Many packaged foods have added phosphorus. Look for phosphorus—or for words with “PHOS”—on ingredient labels.
- Deli meats and some fresh meat and poultry can have added phosphorus. Ask the butcher to help you pick fresh meats without added phosphorus.
| Foods Lower in Phosphorus | Foods Higher in Phosphorus |
|---|---|
|
|
Your health care provider may talk to you about taking a phosphate binder with meals to lower the amount of phosphorus in your blood. A phosphate binder is a medicine that acts like a sponge to soak up, or bind, phosphorus while it is in the stomach. Because it is bound, the phosphorus does not get into your blood. Instead, your body removes the phosphorus through your stool.
Step 5: Choose foods with the right amount of potassium
Why? To help your nerves and muscles work the right way. Problems can occur when blood potassium levels are too high or too low. Damaged kidneys allow potassium to build up in your blood, which can cause serious heart problems. Your food and drink choices can help you lower your potassium level, if needed.
- Salt substitutes can be very high in potassium. Read the ingredient label. Check with your provider about using salt substitutes.
- Drain canned fruits and vegetables before eating.
| Foods Lower in Potassium | Foods Higher in Potassium |
|---|---|
|
|
Some medicines also can raise your potassium level. Your health care provider may adjust the medicines you take.
View tips for people with chronic kidney disease:
- Sodium (PDF, 167.43 KB)
- Phosphorus (PDF, 529.67 KB)
- Potassium (PDF, 158.93 KB)
- Protein (PDF, 1.15 MB)
Preventing Chronic Kidney Disease
You are more likely to develop kidney disease if you have
- diabetes
- high blood pressure
- heart disease
- a family history of kidney failure
What can I do to keep my kidneys healthy?
You can protect your kidneys by preventing or managing health conditions that cause kidney damage, such as diabetes and high blood pressure. The steps described below may help keep your whole body healthy, including your kidneys.
During your next medical visit, you may want to ask your health care provider about your kidney health. Early kidney disease may not have any symptoms, so getting tested may be the only way to know your kidneys are healthy. Your health care provider will help decide how often you should be tested.
See a provider right away if you develop a urinary tract infection (UTI), which can cause kidney damage if left untreated.
Make healthy food choices
Choose foods that are healthy for your heart and your entire body: fresh fruits, fresh or frozen vegetables, whole grains, and low-fat or fat-free dairy products. Eat healthy meals, and cut back on salt and added sugars. Aim for less than 2,300 milligrams of sodium each day. Try to have less than 10 percent of your daily calories come from added sugars.
Tips for making healthy food choices
- Cook with a mix of spices instead of salt.
- Choose veggie toppings such as spinach, broccoli, and peppers for your pizza.
- Try baking or broiling meat, chicken, and fish instead of frying.
- Serve foods without gravy or added fats.
- Try to choose foods with little or no added sugar.
- Gradually work your way down from whole milk to 2 percent milk until you’re drinking and cooking with fat-free (skim) or low-fat milk and milk products.
- Eat foods made from whole grains—such as whole wheat, brown rice, oats, and whole-grain corn—every day. Use whole-grain bread for toast and sandwiches; substitute brown rice for white rice for home-cooked meals and when dining out.
- Read food labels. Choose foods low in saturated fats, trans fats, cholesterol, salt (sodium), and added sugars.
- Slow down at snack time. Eating a bag of low-fat popcorn takes longer than eating a slice of cake. Peel and eat an orange instead of drinking orange juice.
- Try keeping a written record of what you eat for a week. It can help you see when you tend to overeat or eat foods high in fat or calories.
Research has shown that the DASH eating plan NIH external link may help you lower your blood pressure. If you have diabetes, high blood pressure, or heart disease, you may want to locate and work with a dietitian External link to create a meal plan that meets your needs.
Make physical activity part of your routine
Be active for 30 minutes or more on most days. If you are not active now, ask your health care provider about the types and amounts of physical activity that are right for you. Add more activity to your life with these tips to help you get active.
Aim for a healthy weight
The NIH Body Weight Planner is an online tool to help you tailor your calorie and physical activity plans to achieve and stay at a healthy weight.
If you are overweight or have obesity, work with your health care provider or dietitian to create a realistic weight-loss plan. View more weight control and physical activity resources to help you get and stay motivated.
Get enough sleep
Aim for 7 to 8 hours of sleep each night. If you have trouble sleeping, take steps to improve your sleep habits NIH external link.
Stop smoking
If you smoke or use other tobacco products, stop. Ask for help so you don’t have to do it alone. You can start by calling the national quitline at 1-800-QUITNOW or 1-800-784-8669. For tips on quitting, go to Smokefree.gov External link.
Limit alcohol intake NIH external link
Drinking too much alcohol can increase your blood pressure and add extra calories, which can lead to weight gain. If you drink alcohol External link, limit yourself to one drink per day if you are a woman and two drinks per day if you are a man. One drink is:
- 12 ounces of beer
- 5 ounces of wine
- 1.5 ounces of liquor
Explore stress-reducing activities
Learning how to manage stress NIH external link, relax, and cope with problems can improve emotional and physical health. Physical activity can help reduce stress, as can mind and body practices such as meditation NIH external link, yoga NIH external link, or tai chi NIH external link.
Manage diabetes, high blood pressure, and heart disease
If you have diabetes, high blood pressure, or heart disease, the best way to protect your kidneys from damage is to
Keep blood glucose numbers close to your goal. Checking your blood glucose, or blood sugar, level is an important way to manage your diabetes. Your health care team may want you to test your blood glucose one or more times a day.
Keep your blood pressure numbers close to your goal. The blood pressure goal for most people with diabetes is below 140/90 mm Hg. Read more about high blood pressure NIH external link.
Take all your medicines as prescribed. Talk with your health care provider about certain blood pressure medicines, called ACE inhibitors and ARBs, which may protect your kidneys. The names of these medicines end in –pril or –sartan.
Be careful about the daily use of over-the-counter pain medications. Regular use of nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen NIH external link and naproxen NIH external link, can damage your kidneys. Learn more about over-the-counter medicines and your kidneys.
To help prevent heart attacks and stroke, keep your cholesterol levels in the target range. There are two kinds of cholesterol in your blood: LDL and HDL. LDL or “bad” cholesterol can build up and clog your blood vessels, which can cause a heart attack or stroke. HDL or “good” cholesterol helps remove the “bad” cholesterol from your blood vessels. A cholesterol test also may measure another type of blood fat called triglycerides.
Ask your health care provider questions
Ask your health care provider the following key questions about your kidney health during your next medical visit. The sooner you know you have kidney disease, the sooner you can get treatment to help protect your kidneys.
Key questions for your health care provider:
- What is my glomerular filtration rate (GFR)?
- What is my urine albumin result?
- What is my blood pressure?
- What is my blood glucose (for people with diabetes)?
- How often should I get my kidneys checked?
Other important questions:
- What should I do to keep my kidneys healthy?
- Do I need to be taking different medicines?
- Should I be more physically active?
- What kind of physical activity can I do?
- What can I eat?
- Am I at a healthy weight?
- Do I need to talk with a dietitian to get help with meal planning?
- Should I be taking ACE inhibitors or ARBs for my kidneys?
- What happens if I have kidney disease?
What If My Kidneys Fail?
Some people live with kidney disease for years and are able to maintain kidney function. Others progress quickly to kidney failure.
Kidney failure means that your kidneys have lost most of their ability to function—less than 15 percent of normal kidney function. If your kidney function drops to this level, you may have symptoms from the buildup of waste products and extra water in your body.
To replace your lost kidney function, you may have one of three treatment options:
End-stage renal disease (ESRD) is kidney failure that is treated by dialysis or kidney transplant.
Some people with kidney failure choose not to have dialysis or a transplant but continue to receive care from their health care team, take medicines, and monitor their diet and lifestyle choices.
Work with your health care team and family to consider your options and choose a treatment that is right for you.
Clinical Trials for Chronic Kidney Disease
The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) and other components of the National Institutes of Health (NIH) conduct and support basic and clinical research into many diseases and conditions.
What are clinical trials and are they right for you?
Clinical trials are part of clinical research and at the heart of all medical advances. Clinical trials look at new ways to prevent, detect, or treat disease. Researchers also use clinical trials to look at other aspects of care, such as improving the quality of life for people with chronic illnesses. Find out if clinical trials are right for you NIH external link.
Watch a video of NIDDK Director Dr. Griffin P. Rodgers explaining the importance of participating in clinical trials.
Why should i join a clinical trial video link youtube
What clinical trials are open?
Clinical trials that are currently open and are recruiting can be viewed at www.ClinicalTrials.gov